Effective Claim Denial Management for Maximum Revenue
Qbeelmed helps healthcare providers identify, analyze, and resolve claim denials to recover revenue and improve cash flow.
Our expert team proactively manages rejected claims, ensuring compliance, faster resolutions, and optimized revenue cycles.
From denial analysis to appeals, Qbeelmed delivers precise solutions that minimize claim rejections and support smooth billing operations.
Recover Revenue with Expert Denial Management
At Qbeelmed, we specialize in claim rejection and denial management for U.S. healthcare providers. Our certified billing experts thoroughly analyze denied claims, identify root causes, and implement corrective actions to recover lost revenue. By streamlining denial resolution, monitoring payer trends, and optimizing follow-ups, we help practices reduce claim rejections, accelerate reimbursements, and maintain a healthy revenue cycle. Trust Qbeelmed to keep your billing operations efficient, compliant, and revenue-driven.
Grow with Ease
Scale your healthcare practice smoothly and adapt to new payment models at your own pace—without adding staff. Our streamlined revenue cycle processes support sustainable growth while minimizing complexity and overhead, so you can stay focused on long-term success.
Speed Up Getting Paid
Top healthcare providers trust AR Rescue’s RCM services to process claims accurately and efficiently, ensuring faster payments and improved cash flow.
Get your time back
Eliminate the need for additional staff or the time and resources spent training billers. Focus on patient care while we efficiently manage your billing for you.

Numbers That Tell Our Story
” BEHIND EVERY STAT IS A MILESTONE WE ARE PROUD OF “
YEARS IN BUSINESS
CLAIMED PROCESSED
REVENUE IMPROVEMENT
REVENUE IMPROVEMENT
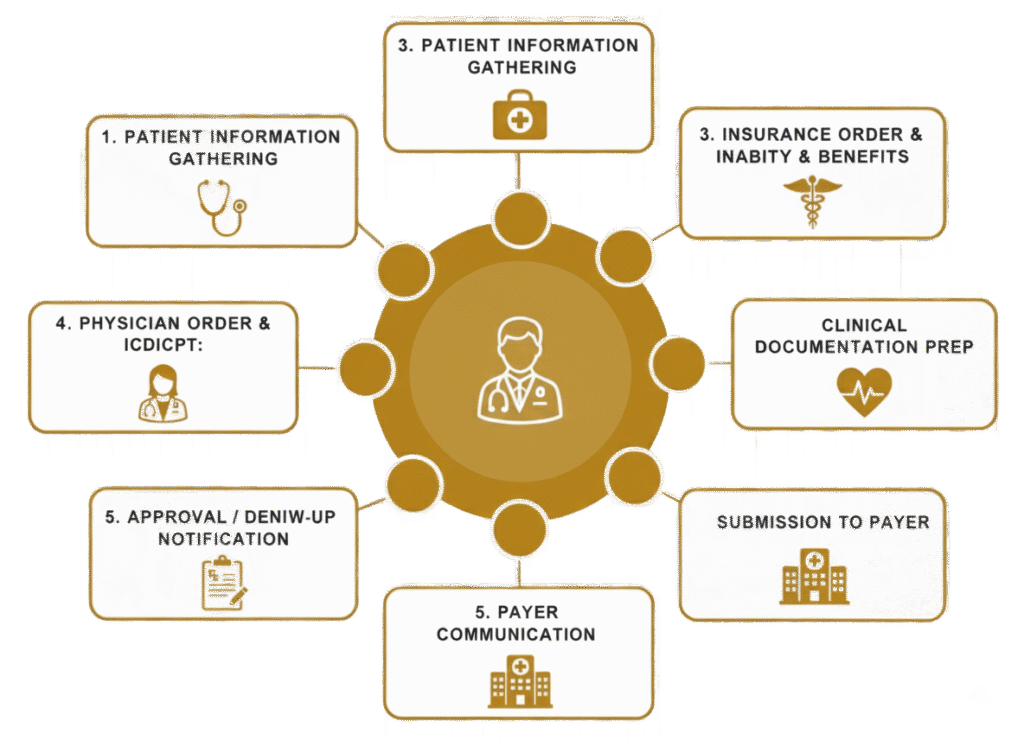
Streamline Denial Management to Recover Lost Revenue
Expert Analysis for Every Denied Claim
At Qbeelmed, we thoroughly investigate every denied or rejected claim to identify the root causes, including coding errors, missing documentation, or payer discrepancies. Our team implements corrective actions to recover lost revenue and prevent recurring denials, ensuring your practice maintains a smooth and efficient billing process.


Proactive Solutions to Minimize Future Denials
Qbeelmed leverages real-time denial trend analysis, payer-specific insights, and automated follow-ups to prevent future claim rejections. By streamlining the appeals process and optimizing denial resolution, we help healthcare providers improve cash flow, reduce administrative burden, and maximize reimbursements.
Boost Your Practice Efficiency Today!
Add our trained Virtual Medical Assistants and focus on what matters—patient care.
